1/51 The young wife is teary eyed. She looks at the husband, as ER docs put him on the ventilator. Heart failing, breathing labored, in shock. The couple did not have children. If he goes, she's alone. Our team was the only one standing between solitude and her beloved.

2/51 Three years back at the age of 35y Shiva developed pain abdomen on the right side along with recurrent bouts of high grade fever and severe itching Paracetamol did relieve the fever, but at the end of it all, he was so tired and his itching gave him sleepless nights
3/51 The first two such episodes, were self limiting over 3 to 5 days. He was wary of hospitals, and so took symptomatic care at home. However, the third fever and abdominal pain episode few months later, shook him to the core. Rigors and chills and he was disoriented.
4/51 Seeing his eyes turn yellow, his wife, Nalini took him to a nearby clinic where they ran tests and told him he had hepatitis and needed higher center care. The itching worsened and insomnia had set in. Shiva was miserable. At a new hospital, the doctors looked at...
5/51 ...his blood work and ultrasound scan of liver. This was exactly something out of the books. They thought. Young male. Recurrent fever. Severe itching. Pain abdomen. Jaundice.

6/51 When there is itching+jaundice, its cholestatic jaundice - which means, jaundice is due to block within the bile ducts that carry bile within the liver or outside the liver. Bile duct block inside liver - intrahepatic cholestasis & outside liver - extrahepatic cholestasis

7/51 There are ways to know clinically, where the block is - inside the liver or outside. Shiva had features of both! Pain Fever (cholangitis - infection/inflammation of ducts) Itching or pruritus The next step was to identify the cause of bile duct block or injury...

8/51 His liver tests showed that he had raised bilirubin, increased fraction of direct bilirubin (meaning it was liver related) and rise in liver enzymes (ALT, AST) ALONG with alkaline phosphatase (ALP) and GGT. Rise in GGT + ALP meant disease was liver related...
9/51 This pattern, where ALP, GGT increase along with jaundice is considered 'cholestatic' or bile duct related liver injury There are many causes for INTRAHEPATIC cholestatic jaundice - commonly infections, alcohol, recent drugs (anabolic steroids, antibiotics, herbal agents)

10/51 The EXTRAHEPATIC cholestatic jaundice causes include mainly bile duct stones and various types of cancers affecting liver and bile ducts, and also - disease of the pancreas leading to shrinkage of bile ducts or tumor of pancreas causing block of bile ducts.

11/51 Further diagnosis required the doctors follow an algorithm. According to the algorithm, cholestatic pattern of jaundice required the next best step to be ultrasound of liver - to look for obstructions inside or outside the liver - stones, tumors, pancreas disease etc.

12/51 In Shiva's case, the ultrasound showed that bile ducts were shrunken as well as dilated at certain places both inside and outside the liver Along with clinical and blood findings, in the absence of stones, large cancers and presence of...

13/51 ...bile duct issues both inside and outside the liver, in a young man, the only diagnosis was thought of - pending confirmation. Primary sclerosing cholangitis or PSC is a terrible disease affecting young men where bile ducts undergo inflammation, damage and shrinkage...

14/51 ...leading to bile getting held up inside the liver, causing liver inflammation, progressive damage and cirrhosis in long term. The cause is multiple - from genetics to immune disorder to environmental factors.

15/51 To confirm, we needed to do a MRCP - a MRI of the bile ducts to see for strictures or bile duct shrinkage/narrowing (inside and/or outside the liver) This was almost conclusive because other causes of cholestatic jaundice came back negative. MRCP showed severe...

16/51 ...stricturing, narrowing, beading and dilatation of bile ducts both inside and outside, which was highly suggestive of PSC. However, there were other diseases that could look the same and hence, a liver biopsy was the final diagnosis in this matter.

17/51 And so a biopsy was ordered and the results fit perfectly with the diagnosis of PSC. The classical biopsy feature is onion-skin layered scarring appearance around thickened bile ducts as shown below


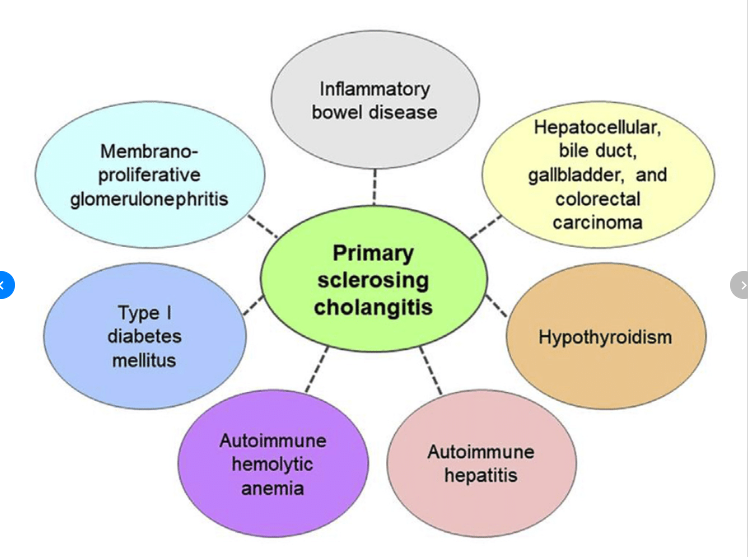
18/51 The next step was to find OTHER organ systems disease associations with PSC. Many organ systems are affected and the commonest among them is the large bowel - a condition called inflammatory bowel disease - ulcerative colitis type. A colonoscopy showed that Shiva had...
19/51 ...mild colitis which was also confirmed on colon biopsy. So the doctors needed to treat Shiva. PSC is a disease without a cure - one has to control symptoms, prevent disease progression and halt life threatening complications such as recurrent infections due to bile...

20/51 ...block, bile duct cancers, large dominant stricture formation, stone formation, cirrhosis development and liver failure. This requires another strategic approach. Risk - stage - manage - surveillance. And so they start.

21/51 Clinically it was important to differentiate PSC from another similar looking disease called PBC or primary biliary cholangitis, which was seen more in women. Rarely, patients can have both, called PSC-PBC overlap syndrome, which can also occur with autoimmune hepatitis.

22/51 It is important that patients with PSC be screened and undergo surveillance for a variety of cancers, most critically, bile duct cancer or cholangiocarcinoma. The doctors put Shiva on a surveillance protocol.

23/51 Unfortunately, there is no approved treatment for PSC. The commonly used drug is ursodeoxycholic acid or UDCA at 8 mg/kg body weight per day in divided doses. Combination with steroids, antibiotics (especially when associated with repeat infections) have shown some...
24/51 ...benefit, but none to comprehensively reverse damage or halt progression. So multiple types of treatments have to be decided based on disease condition, associated non-liver issues and complications. However, the biggest issue Shiva faced was recurrent infections...

25/51 ..in the absence of dominant strictures - that is a major block in the bile duct which can be easily smoothened and removed using an endoscopic procedure called ERCP. But Shiva did not have a major stricture, he had multiple small ones, leading to repeated infections.

26/51 The docs were unable to improve Shiva's clinical status, he was referred to us for advanced care. Diagnosis of PSC was confirmed. But Shiva was sick. He was initially febrile, with pain abdomen and jaundice and later on developed altered behavior, low blood pressure.

27/51 In 1877, a French physician Jean-Martin Charcot described jaundice, pain and fever in patients - calling it 'hepatic fever' - which was later found to be 'acute cholangitis' - an infection due to stagnation of bile in bile ducts - it came to be known as Charcot's Triad..
28/51 ..in 1959, Dr. Benedict Reynolds and his colleague Dr. Everett Dargan found that when patients with Charcot's triad developed confusion+low BP (hypotension) - it was associated with worse clinical outcomes. This additional description came to be known as Reynold's Pentad.

29/51 When patients present with acute cholangitis (infection of bile ducts) we follow an algorithm Medicine was nothing but evidentiary, tested knowledge systematically applied for the good of mankind. Since Shiva did not have major obstructions, antibiotics were started.

30/51 BUT, repeated infections(called recurrent cholangitis)was one of the bad factors in PSC - this would mean that death could come early. With repeated infections and repeated antibiotic use, more and more resistant bacteria would form and patients would die of severe..
31/51 ...infections not responding to high end antibiotics and multiple organ failure. Shiva already had 2 severe infections and the third one had landed him in the ICU on the ventilator because he developed septic shock - a forerunner of multiple organ failure. There was...

32/51 ..very little from medical therapy one could do. Except one thing A liver transplant In PSC, repeated infections, among others, was indication for transplant. But there was a problem Shiva had only Nalini & Nalini, Shiva They dint have children, they married late..

33/51 ..and so liver donation was not possible as the family did not have close relatives to donate and Nalini did not match. The whole aspect now came down to best supportive care - but Shiva had to get out of this critical infection first, for us to plan something to..
34/51 ..to prolong his life. In the ICU the critical care specialists throw everything they have at the bugs that are killing Shiva. They are in his blood. They are streaming inside him. Multiple antibiotics are used and finally, Shiva's heart functions start improving.
35/51 How does one cope with an unexpected death? How does one feel when a beloved family member is lost, suddenly? What if there is no time to prepare for grief? All of these thoughts went through my head - because one thing was sure. I had to prepare Nalini...

36/51 ..for Shiva's death in the very near future. But I did not know how. Slowly, but steadily, Shiva started getting better. His infections were getting controlled. His ventilator requirements came down and he started to wake up. In a matter of 8 days, he was out of...
37/51 ...the ventilator and inside the room, where he saw Nalini after what felt like a whole year for him. They were close. Very close. Because they had only each other. Three days before discharge, I spoke to both regarding what the future held. Shiva was not ready for it...
38/51 ..he broke down. Nalini was strong, because she still thought he was going to be ok. Infections will come and go and things will be the same. There had to be something. Additional experimental drugs were not useful. Shiva would not tolerate immunosuppression drugs as...
39/51 ..they would cause more infection complications in him. What was left? And we started looking at new targets to hit at, in PSC - to improve patient survival and came across something that was just emerging as playing important role in PSC. The intestinal bacteria.

40/51 From year 2015 to 2017 ---> 5 groups of doctors had identified that intestinal bacteria in PSC patients were very different and of the harmful to host. https://t.co/pLPH0q7KM9 But none had actually attempted to modulate it and see what happens to the PSC patients.
pubmed.ncbi.nlm.nih.gov/29272894/

41/51 There was ample evidence, that in severe large bowel infections, alcohol-hepatitis and inflammatory bowel disease - changing the bad bacteria in the intestine, through stool transplant would help patients. This was also possible in PSC patients - but none had done it.

42/51 So before discharge, I spoke to Shiva and Nalini and tell them about healthy donor stool transplant. We did not have any protocol - so we made one for Shiva - we would give him fresh stool transplant from a healthy donor - every week once, for 4 weeks via an endoscope.
43/51 Shiva and Nalini looked at me for a while, astonished at this therapy and then without hesitating, nodded their heads. Shiva would be discharged, they would find a stool donor and we would start within a week After a week, Shiva comes in with his niece and she clears..
44/51 ..the screening for stool donation and we begin. Through an endoscope, we push in 200ml of freshly made stool suspension into a sedated Shiva once weekly for 4 weeks. We check his liver tests and chances of infections. To our great astonishment, it paid off.

45/51 Through high end analysis methods, we found that the donor stool bacteria were overwhelming the bad bacteria inside Shiva's intestines And in due to course, they took over completely annihilating the bad bacterial groups, there by reducing Shiva's infection complications.

46/51 During the time of stool transplant and 1 year there after, Shiva remained fever free and his liver tests remained stable. This was something new. We had done it. The 1st stool transplant for PSC in a patient who needed transplant and was dying due to repeated infections.
47/51 We published the first report of stool transplantation to control severe infections in PSC patients shortly thereafter (pic) After our report was published, a US group performed stool transplant for PSC and found it safe and improved liver tests -
pubmed.ncbi.nlm.nih.gov/30730351/

48/51 There was something more. During one follow up, Shiva came to the OPD with his cousin. Nalini was missing for the first time. He gladly tells me, she was pregnant. And how they were excited. It was happiness all around. They got me sweets. And I wished them the best.
49/51 However, at the end of one year, Shiva started developing jaundice again. The effects of the stool transplant started to wean off. Nalini wanted to try stool transplant again, but Shiva wanted a permanent solution. Because they could save money, he was worked up & put..
50/51 ..on the cadaver liver list, waiting for brain dead voluntary donation. Shiva survived longer than was expected - with repeated infections/hospitalizations but none severe except the last one More than 2y after the stool transplant, Shiva died in my unit from a severe..
51/51 ..bout of infection and massive blood vomiting. Nalini knew we had done everything for him. She was within him when he passed away. But this time, she was not alone. Her little daughter waited for her mother, outside the ICU, while she said her last goodbye to Shiva.

